What Is AMR? Understanding the Growing Threat of Antimicrobial Resistance
The question what is AMR has become one of the most urgent in global health today. AMR stands for antimicrobial resistance — a complex and growing problem that threatens the effectiveness of life-saving medicines used to treat infections. In simple terms, AMR happens when microbes such as bacteria, viruses, fungi, or parasites evolve to resist the drugs that were once effective against them.
But what is AMR beyond the definition? It's a major public health challenge that affects how we treat common infections, how safe surgeries and medical procedures are, and even how long people live. Understanding what AMR is, why it happens, and what we can do to stop it is essential for individuals, healthcare professionals, and policymakers alike.
Why It Matters to Ask "What Is AMR"
Asking what is AMR is not just about understanding a scientific term — it's about facing a crisis that affects us all. Antimicrobial resistance is growing rapidly across the globe and poses a serious threat to human and animal health. If left unchecked, AMR could make even routine infections deadly and undermine decades of progress in modern medicine.
In many countries, including Nigeria, AMR is already impacting healthcare systems. Infections that were once easy to treat now linger longer, require more expensive medications, and sometimes don't respond to treatment at all. The rise of AMR means increased healthcare costs, longer hospital stays, and higher mortality rates.
What Causes AMR?
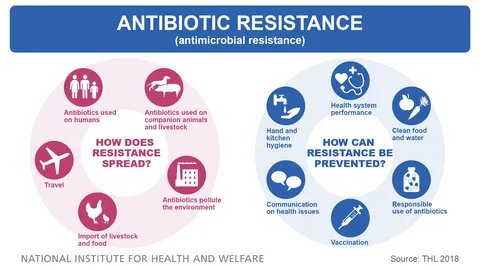
To fully understand what is AMR, we need to explore what causes it. Microbes are constantly changing and adapting, and they can develop resistance to the drugs meant to kill them. Here are the most common drivers of antimicrobial resistance:
Misuse and Overuse of Antimicrobials
Taking antibiotics when they are not needed, using them to treat viral infections like the flu, or not completing a prescribed course allows microbes to survive and adapt.
Use of Antibiotics in Animals
In agriculture, antibiotics are often used to promote growth or prevent disease in animals — even when they’re not sick. This can lead to the development of resistant bacteria that can be transferred to humans through food or the environment.
Poor Infection Prevention and Control
Weak sanitation, lack of clean water, overcrowded health facilities, and insufficient infection control practices make it easier for resistant microbes to spread.
Lack of Awareness
Many people don’t know what AMR is or how their actions can contribute to it. Public education is a key part of controlling resistance.
Inadequate Surveillance and Diagnostics
Without strong laboratory systems and diagnostic tools, healthcare providers often prescribe antibiotics blindly, increasing the chance of misuse.
How Does AMR Work?
When exploring what is AMR, it’s important to understand how resistance develops. Microorganisms can become resistant in several ways:
Mutation: Microbes may change their genetic structure, making the drug ineffective.
Gene Transfer: Bacteria can share resistant genes with other bacteria, even across species.
Enzyme Production: Some microbes produce enzymes that neutralize the antibiotic.
Biofilm Formation: Microbes can form protective layers, making it difficult for drugs to penetrate and work effectively.
These changes allow microbes to survive even in the presence of medicines designed to destroy them.
The Consequences of AMR
The implications of AMR are wide-ranging and severe. When you understand what is AMR, it becomes clear how dangerous it can be:
Treatment Becomes More Difficult: Infections that were once easily cured now take longer to treat and may require multiple medications.
Increased Death Rates: Common infections could become fatal if drugs stop working.
Longer Hospital Stays: Patients with resistant infections often need more extended care.
Higher Medical Costs: Stronger, more complex drugs are often more expensive and harder to access.
Threats to Modern Medicine: Surgeries, chemotherapy, and organ transplants depend on effective antibiotics. Without them, these procedures become riskier.
What Is AMR in the Nigerian Context?
In Nigeria, AMR has become a growing concern. Inappropriate use of antibiotics, weak regulatory enforcement, and limited access to proper diagnostics have accelerated resistance. This is why national efforts, like those led by the Nigeria National Antimicrobial Stewardship Technical Working Group (NNAST), are so vital.
These efforts focus on promoting antimicrobial stewardship, improving laboratory capacity, raising public awareness, and supporting research to fight resistance. Understanding what is AMR helps build a more informed and proactive health system.
How Can We Combat AMR?
Fighting AMR requires a coordinated and multi-sectoral approach. Here's how we can respond:
Antimicrobial Stewardship
This means using antimicrobials only when necessary, at the right dose, and for the appropriate duration. Healthcare providers play a key role in this effort.
Improved Diagnostics
Rapid, affordable, and accurate testing helps doctors prescribe the correct treatment, reducing unnecessary drug use.
Public Awareness Campaigns
Educating the public about what AMR is and how to prevent it is crucial. This includes encouraging good hygiene, handwashing, and the responsible use of medicine.
Stronger Regulations
Governments must regulate the sale of antimicrobials, monitor resistance patterns, and ensure only quality-assured medicines are available.
One Health Approach
Since human, animal, and environmental health are interconnected, addressing AMR requires collaboration across all sectors — from hospitals to farms to water systems.
Your Role in Preventing AMR
Once you understand what is AMR, you can take simple actions that make a big difference:
Do not self-medicate. Always get a prescription from a qualified healthcare provider.
Finish your treatment. Never stop taking antibiotics halfway, even if you feel better.
Never share antibiotics. Medications should be used only by the person they are prescribed for.
Practice good hygiene. Preventing infections reduces the need for antibiotics.
Support awareness campaigns. Spread the message about AMR in your community.
Conclusion: Why Understanding What Is AMR Matters
So, what is AMR? It is the ability of microbes to resist the medicines that once killed them — but it’s also much more than that. AMR is a global health emergency that affects everyone, from patients in hospitals to farmers in rural areas. It threatens the effectiveness of modern medicine, puts millions of lives at risk, and increases the burden on healthcare systems.
By understanding what AMR is and why it happens, we can take action to protect our health and our future. Governments, healthcare professionals, scientists, farmers, and individuals must all work together to slow the spread of resistance. Because the fight against AMR begins with knowledge — and that starts by asking the right question: what is AMR?